A new study might found the reason why COVID-19 is so challenging to treat. In the study conducted by the Purdue University, scientists found that the virus triggered a biochemical pathway known as the immune complement system in the lungs.
According to scientists, pairing antiviral drugs with drugs that inhibit this process may be more effective.
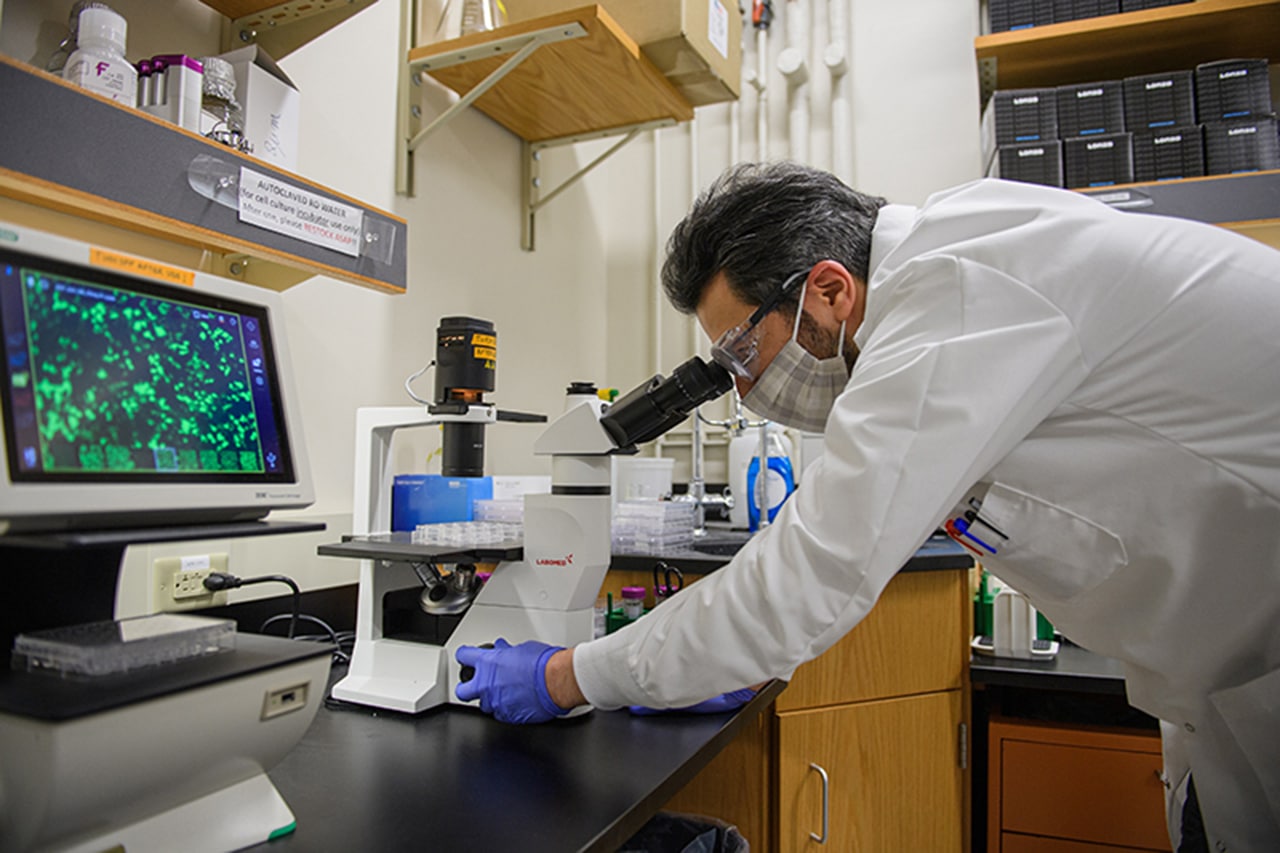
For the study, scientists used in vitro model using human lung cells. They found that the antiviral drug Remdesivir in combination with the drug Ruxolitinib inhibited this complement response.
Majid Kazemian, assistant professor in computer science and biochemistry at Purdue University, said, “We examined more than 1,600 previously FDA-approved drugs with known targets. We looked at the up-regulated genes by COVID-19 but down-regulated by specific medications, and Ruxolitinib was the top drug with that property.”
“The immune complement system is a complex system of small proteins produced by the liver that aids or complements the body’s antibodies against blood-borne pathogens. Surprisingly, scientists discovered that this complement response is triggered in cells of the lungs’ small structures known as alveoli.”
Kazemian said, “We observed that SARS-CoV2 infection of these lung cells causes an activated complement system’s expression in an unprecedented way. This was entirely unexpected for us because we were not thinking about activating this system inside the cells, or at least not lung cells. We typically think of the complement source as the liver.”
Claudia Kemper, senior investigator and chief of the Complement and Inflammation Research Section of the National Institutes of Health, said, “The complement system is traditionally considered a liver-derived and blood-circulating sentinel system that protects the host against infections by bacteria, fungi, and viruses. It is unexpected that in the setting of a SARS-CoV2 infection, this system instead turns against the host and contributes to the detrimental tissue inflammation observed in severe COVID-19. We need to think about the modulation of this intracellular, local complement when combating COVID-19.”
Dr. Ben Afzali, an Earl Stadtman Investigator of the National Institute of Health’s National Institute of Diabetes and Digestive and Kidney Diseases, said “there are now indications that this has implications for difficulties in treating COVID-19.”
“These findings provide important evidence showing not only that complement-related genes are amongst the most significant pathways induced by SARS-CoV2 in infected cells, but also that activation of complement occurs inside of lung epithelial cells, i.e., locally where the infection is present.”
“This may explain why targeting the complement system outside of cells and in the circulation has, in general, been disappointing in COVID-19. We should probably consider using inhibitors of complement gene transcription or complement protein activation that are cell-permeable and act intracellularly instead.”
Afzali cautions that appropriate clinical trials should be conducted to establish whether a combination treatment provides a survival benefit.
“The second finding that I think is important is that the data suggest potential benefit for patients with severe COVID-19 from combinatorial use of an antiviral agent together with an agent that broadly targets complement production or activation within infected cells.”
“These data are promising, but it is essential to acknowledge that we carried out the drug treatment experiments in cell lines infected with SARS-CoV2. So, in and of themselves, they should not be used to direct the treatment of patients.”
Journal Reference:
- Bingyu Yan et al. SARS-CoV-2 drives JAK1/2-dependent local complement hyperactivation. DOI: 10.1126/sciimmunol.abg0833
Continue reading COVID-19 triggers a biochemical pathway in the lungs on Tech Explorist.
0 comments:
Post a Comment